50/M PTB HBSAG
50/M CAME WITH
CHIEF COMPLAINTS:
c/o cough since 20 days
c/0 SOB since 20 days
c/o fever since 7 days
HISTORY OF PRESENT ILLNESS
Pt was apparently asymptomatic 20 days back then
1.he developed cough with sputum, mucopurulent, non blood stained ,non foul Smelling, more cough during night,
- no seasonal variation, not associated with chills.
- no aggrevating & relieving factors
2.c/o SOB since 20 dats
- Grade II (MMRC),
- not associated wheeze,
- no aggravating no seasonal variation,
- more during Early mornings.
- no aggravating & relieving factors, no orthopnea, no PND.
3.c/o fever since 7 days
- intermittent type, Low grade fever
- relieved of medication. & rigors,
- no Evening rise of temperature
4.clo wt loss and loss of appetite from 4 months no c/i Chest Pain Chest fightness, hemoptysis, palpitations
5.h/0 Similar complaints 4 months back.
h/o of TB 4 months back (detected in sputum CBNAAT) H/O TB AAT (3 tabs/day) for 2 months, then stopped
PAST HISTORY
not a known case of CAD,CVD, thyroid disorders epilepsy
No history of surgeries
PERSONAL HISTORY :
- Diet: mixed
- Appetite: increased
- Bowel habits: normal
- Bladder habits: normal
- Sleep: normal
- Addictions:
(i) alcohol consumption - daily 180ml
stopped from 6months
(ii) smoker since 30 years - 2 pack of beedi/day
stopped from 6months
FAMILY HISTORY :
not significant
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative.
Examined after taking valid informed consent in a well enlightened room.
- Pallor - absent
- Icterus - absent
- Clubbing -absent
- Lymphadenopathy - absent
- Cyanosis - absent
- Pedal edema -absent
VITALS :
- Temperature: 101F
- Pulse : 130 bpm
- Respiratory rate : 20 per minute
- Bp 110/70
- Spo2 96%
- GRBS 105 mg%
CVS EXAMINATION
S1 S2 heard
no murmurs
RESPIRATORY SYSTEM
Bilateral air entrty present
NVBS
PER ABDOMEN
soft, non tender
URT
- Nose - No DNS, No nasal polyps.
- Oral cavity - normal oral hygeine
- Dental Carier +
- Posterior pharyngeal wall - normal
LRT
1.inspection
- Shape of chest - Elliptical
- B/L symmetrical
- Trachea appears to be central (Trail's sign - Absent)
- Chest Expansion - Equal on BS.
- usage of accessory muscles of respiration
- left supra clavicular hollowness > right supraclavicular hollowness
- crowding of ribs + left side > R
- NO drooping of Shoulders.
- Spino scapular distance L>R
- Apical impulse not seen
- wasting of muscles +
- No kyphosis & scoliosis
- Skin over chest - no sinuses, scars, engorged veins
2. palpation
- All inspectory finding conformed
- No local rise
- No tenderness
- Trachea slightly deviated to left
- chest morte slightly decreased left-side
- Ape beat - left 5th ICS medial to MCL
- TVF- equal on BS
- AP diameter -20cms
- Transverse - 24cm
- CC - inspiration : 80 cm
- expiration : 79cm
- right hemi - 42cm
- left hemi - 40 cm
3. percussion
- direct - resonant
- indirect - resonant in all areas
- liver dullness : from right 5th ICS
- cardiac dullness : within normal limits
4. auscultation
- BAE +
- decreased BS in left ICA, infra SA, IAA
- crepts + left ISA
- VR - equal on BS
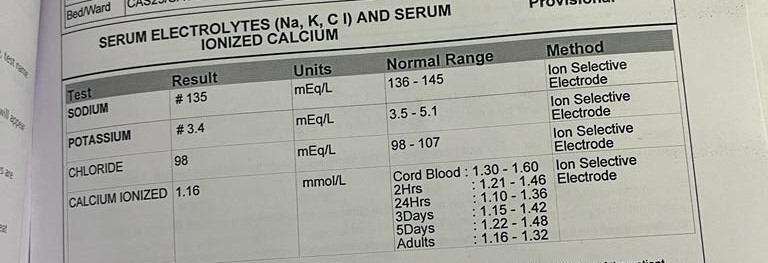
INVESTIGATIONS :
PROVISIONAL DIAGNOSIS:
left FIBRO CAVITARY DISEASE SECONDARY to TB WITH HbsAg +
TREATMENT GIVEN
1) INJ. CEFTRIAXONE 1 GM IV BD FOR 5DAYS
2) INJ PAN 40 MG IV ODFOR 5DAYS
3) TAB PCM 650 MG PO TID IF TEMP >99 F
4) TAB MVT PO/ OD
5) SYP. ASCORIL LS 2TSP PO /TID
2) INJ PAN 40 MG IV ODFOR 5DAYS
3) TAB PCM 650 MG PO TID IF TEMP >99 F
4) TAB MVT PO/ OD
5) SYP. ASCORIL LS 2TSP PO /TID
6) TAB MUCINAC 600MG PO BD(MIX IN 1 GLASS OF WATER)
7) PROTEIN POWDER 2 TSP IN 1 GLASS OF WATER BD
8) 2 EGG WHITES PER DAY
9) ATT (3TABS/DAY) BBF PO UNDER NTEP (IP) DAY 1
7) PROTEIN POWDER 2 TSP IN 1 GLASS OF WATER BD
8) 2 EGG WHITES PER DAY
9) ATT (3TABS/DAY) BBF PO UNDER NTEP (IP) DAY 1
Sputum afb seen , sputum cbnaat positive
Att started on 14-2-2023 AND HE COMPLETED TREATMENT IN AUG 2023 AND WAS FOUND TO BE SPUTUM NEGATIVE. CONTACTED HIM IN SEPT 2023
OUTCOME- COMPLETELY RECOVERED











Comments
Post a Comment