60 M ?TB MENINGITIS RVD
A 60 year old male who is a resident in telangana ,he does a cotton business. Came to the casualty in altered sensorium on 30/04/2023.
Patient was apparently asymptomatic 10 years back then he developed fever and went to a ayurvedic doctor and was found to be having retroviral postive.
And started using herbal medicine for that and the symptoms he was experiencing back then was subsided.
1month back patient developed weakness in his left hand with tingling and numbness sensation which is insidious in onset and gradually progressive in nature with no aggravating and releiving factors for that he visited the same previous Ayurveda doctor and started using some herbal medicine prescribed by him and then, 3to 4 days later, he developed fever (on and off) and no chills and rigors, which is insidious in onset and gradually progressive in nature along with the fever he also started experiencing leg (both the legs)pain and weakness as well as flank pain for which he went to the same Ayurvedic doctor and he got a scan done the doctor told him that he had stones in his kidneys and prescribed some herbal medicine with dolo and multivitamin tablets. But after this also the fever did not subsided so they again went to him (Ayurvedic doc) 10 days back and the doctor adviced some investigations and after that he told that his viral load is high and prescribed herbal medicine which are of high dose and after using this high dose herbal medicine for 4 to 5 days the patient developed dysphagia and pain in the throat which is insidious in onset and gradually progressive in nature (dysphagia initially to solids and then later to liquids).
He also developed cough 4 days back which is insidious in onset and gradually progressive in nature no history of weight loss,no history of night sweats and after that his responsiveness was decreased and now presented with altered sensorium.
PSYCHOSOCIAL HISTORY: This patient has a friendly relationship with his family friends as well as neighbors
PAST HISTORY:
Know case of HIV POSTIVE since 10 years
Known case hypertensive since 3 years.
Not a known case of DM2,ASTHMA,EPILEPSY,TB,CAD.
DAILY ROUTINE:
He does cotton business.
He daily wakes at 5 Am and takes bath and fresh up drinks tea at 7am and then he takes his breakfast (RICE with vegetable curry )at 8am and goes for his business and comes at 1 pm and takes his lunch which consisting of a vegetable curry and rice and after his lich he chit chat with his neighbors and lie down for some time and after that he watch TV and then eats his dinner at 8pm and goes to sleep at 9pm.
Family history:No similar complaints in the family .This old man has 4 childern(2 sons and 2daughters) and his wife died 5 years ago due to some health issues.
PERSONAL HISTORY:
DIET:VEGETERIAN
APPETITE:DECREASED SINCE 2 MONTHS
BOWEL BLADDER :NOT PASSING STOOLS SINCE 4 DAYS.
SLEEP:ADEQUATE
ADDICTIONS:HE STARTED TAKING BEER 15 DAYS BACK FROM THIS ILLNESS FOR 10 DAYS.
GENERAL EXAMINATION:
Patient is drowsy but arousal.
GCS:E2V1M5
BP:130/80mmhg.
PR:110/min
RR:18CPM
SPO2:95%ON 8 LIT OF O2
TEMP: 99°F
PALLOR PRESENT,no icterus,cyanosis,clubbing,lymphadenopathy and edema
SYSTEMIC EXAMINATION:
CVS:S1,S2 HEARD,NO MURMURS.
RS:BAE+,NVBS.
PA:SOFT AND NONTENDER
CNS:PUPILS :NORMAL SIZE AND NON REACTIVE.
TONE: RT. LT
UL HYPER. HYPER
LL HYPER. NORMAL
POWER:
UL 2/5. 2/5
LL 2/5. 2/5
REFLEXES:
B: 3+ 3+
T: 2+ 2+
S: 2+ 2+
K: 2+ 3+
A: 1+ 1+
P: EXTENSORS
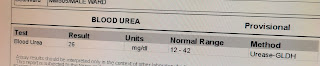
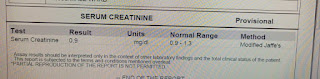
CLINICAL IMAGES AND INVESTIGATIONS
30/04/23
S:
5 FEVER SPIKES SINCE YESTERDAY 8AM
STOOLS NOT PASSED .
O:
On examination
Patient is drowsy but arousal.
GCS:E1V1M3
BP:110/80mmhg.
PR:140/min
RR:22CPM
SPO2:95%ON 8 LIT OF O2
TEMP: 98°F
CVS:S1,S2 HEARD,NO MURMURS.
RS:BAE+,NVBS.
PA:SOFT AND NONTENDER
CNS:PUPILS :DOLLS EYE+
PUPILS NORMAL SIZE AND NON REACTIVE TO LIGHT.
TONE: RT. LT
UL HYPER. HYPER
LL HYPER. HYPER
POWER:
UL 2/5. 0/5
LL 2/5. 0/5
REFLEXES:
B: 2+ 2+
T: 2+ 2+
S: 2+ 2+
K: 2+ 3+
A: 1+ 1+
P: EXTENSORS
A:
ALTERED SENSORIUM 2°TO ?MENINGITIS,2°TO ?TB,?ACUTE ISCHEMIC STROKE. RETROVIRAL POSTIVE (10 YEARS)WITH KNOWN HYPERTENSIVE SINCE 3 YEARS .
P:
RYLES FEEDING :100ML OF WATER EVERY 2ND HOURLY.
200ML OF MILK EVERY 4TH HOURLY.
IVF:NS@75ml/hr.
Inj.NEOMOL. 1gram IV/SOS. IF TEMP IS greater than 101°F.
SUCTION 2ND HOURLY.
MONITORING VITALS HOURLY
S:
3 FEVER SPIKES SINCE YESTERDAY 8AM( at 4pm,5pm,10pm)
STOOLS NOT PASSED .
O:
On examination
Patient is drowsy but arousal.
GCS:E2V2M3
BP:130/90mmhg.
PR:98/min
RR:26CPM
SPO2:96%ON 8 LIT OF O2
TEMP: 98°F
CVS:S1,S2 HEARD,NO MURMURS.
RS:BAE+,NVBS.
PA:SOFT AND NONTENDER
CNS:PUPILS :DOLLS EYE+
PUPILS NORMAL SIZE AND NON REACTIVE TO LIGHT.
TONE: RT. LT
UL HYPER. HYPER
LL HYPER. HYPER
POWER:
UL 2/5. 0/5
LL 2/5. 0/5
REFLEXES:
B: 1+ 1+
T: 1+ 1+
S: 1+ 1+
K: 1+ 1+
A: 1+ 1+
P: EXTENSORS
A:
ALTERED SENSORIUM 2°TO ? TB MENINGITIS,RETROVIRAL POSTIVE (10 YEARS)WITH KNOWN HYPERTENSIVE SINCE 3 YEARS .
P:
RYLES FEEDING :100ML OF WATER EVERY 2ND HOURLY.
200ML OF MILK EVERY 4TH HOURLY.
IVF:NS@75ml/hr.
Inj.NEOMOL. 1gram IV/SOS. IF TEMP IS greater than 101°F.
TAB:ISONIAZID 5mg/kg.PO/OD
Tab:RIFAMPICIN 10mg/kgPO/OD
TAB;PYRAZINAMIDE 25mg/kgPO/OD
TAB:ETHAMBUTOL 15mg/kg PO/OD
TAB:BENADON 40mg po/OD
INJ:DEXA 6mg iv/tid
Inj:PANTOP 40mg iv
SUCTION 2ND HOURLY.
MONITORING VITALS HOURLY.
wats app pajr group discussion online learning :
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4913673/
Early initiation of ART within 8 weeks of ATT or within 2–4 weeks is associated with a lower risk of mortality, especially among those with low CD4 cell counts, even though there is a higher risk of immune reconstitution inflammatory syndrome
shared by DR.KEERTHI PGY2
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606267/
Tuberculous meningitis (TBM) is still a crippling disease with a high degree of morbidity and mortality. One of the most severe complications of TBM is stroke resulting from vascular involvement. In HIV-infected individuals with TBM, the immune response to the tuberculous bacilli is altered; therefore, pathological features are very different from those seen in patients with relatively normal cell-mediated immunity (CMI). The brains of such individuals showed minimal inflammatory response with parenchymal infarcts and vasculitis, not only in the basal ganglia but in the cortical parenchyma as well.
SHARED BY DR.keerthi PGY2
Let's cover him for streptococcus pneumonia as well as PCP
Share the literature on drug choice and efficacies
The mainstay of treatment for patients with S. pneumonia is antibiotic therapy and supportive care including mechanical ventilation if necessary. Treatment of CAP varies based on the area of practice and severity of the disease. Patients with low-risk CAP are typically treated as an outpatient with macrolide monotherapy. Respiratory fluoroquinolones are used in outpatient patients at higher risk. Non-ICU inpatients are treated with a dual therapy of a b-lactam plus a macrolide or respiratory fluoroquinolone monotherapy.
for PCP
the first-line treatment choice for HIV-infected and uninfected patients is 21 days of trimethoprim-sulfamethoxazole (TMP-SMX).[17] For mild to moderate treatment, TMP 15 to 20 mg/kg/day and SMX 75 to 100 mg/kg/day, given orally in 3 or 4 divided doses or TMP-SMX DS, two tablets three times per day. For moderate to severe cases (e.g., PaO ≤ 60 mmHg, respiratory rate > 25), TMP 15 to 20 mg/kg/day and SMX 75-100 mg/kg/day are given intravenously (IV) every 6 to 8 hours with a switch to oral when the patient shows clinical improvement. In patients with a mild allergy to TMP-SMX, desensitization should be attempted as this is the most effective drug of choice. In patients with severe allergies to TMP-SMX, desensitization is no longer recommended, and choosing a different drug regimen is more appropriate.
SHARED BY DR.keerthi PGY2













































.jpg)
























Comments
Post a Comment